Family health insurance premiums hit another record: $26,993
Published in Business News
The price tag of health insurance from employers keeps getting bigger across the U.S., and the increases this year are fueling concerns over medical spending across all health insurance markets.
The average annual premium for family health insurance rose about 6% this year to nearly $27,000, according to widely watched survey results released Wednesday by KFF, a California-based health care research group.
Most of that price is typically paid by employers and is thus less visible to the consumer.
The average premium, which is roughly equivalent to the base price of a 2026 Subaru Crosstrek, grew by $1,408 compared with last year. And price growth is widely expected to be even more stark in 2026.
New weight loss drugs, higher hospital prices and a host of other factors such as tariffs are driving costs higher.
Some of those same forces are being blamed for sharp price increases in Medicare coverage and individual policies next year.
The annual report on employer-sponsored coverage, which gauges the already burdensome weight of financing the nation’s health care system, suggests the load for employers and families will only get heavier, since the nation lacks new strategies for containing costs.
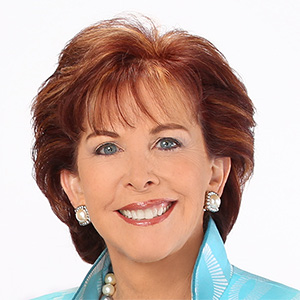
“There is a quiet alarm bell going off,” Drew Altman, the president of KFF, said in a statement. “We expect employer premiums to rise more sharply next year.”
The survey analyzes trends in the market for employer-sponsored coverage, which insures about 154 million Americans and is the largest source of insurance across the country.
In 2023, about 49% of Minnesota residents were covered through job-based health plans.
The report did not describe trends at the state level, but employers in Minnesota say they’re feeling the pain.
“We find about three-quarters of our folks who offer insurance say: These cost pressures are unsustainable,” said Bentley Graves, director of health care and transportation policy at the Minnesota Chamber of Commerce.
Earlier this month, Minnesota announced double-digit premium increases next year for people who buy health insurance on their own. Premiums for small employers, with two to 50 workers, are increasing an average of 14.2%.
The federal government is projecting the average Medicare Advantage insurance premium for Minnesotans will increase nearly 18% next year, unlike the projected declines in premiums across the country.
“What you’re seeing is these different markets and the financial pressures being pushed throughout,” said Lucas Nesse, president and chief executive of the Minnesota Council of Health Plans, a trade group for nonprofit health insurers in the state.
The problem might get worse for employers due to future federal reductions in coverage via Medicaid, the state-federal program for lower-income residents.
Nesse said health care providers already are sizing up the Medicaid cuts, which mostly kick in during 2027, and arguing to insurers that they need to make up the difference via even higher reimbursements from employer health plans.
The impact of already high prices, he said, is being magnified by higher use of health care services, pushing overall costs to a new level.
The KFF survey found that, across the country, workers on average are contributing $6,850 this year — about one quarter of the total $26,993 average premium — for family coverage, a similar share to 2024. Employers are paying the rest, an average of $20,143.
The increase in average family premiums this year is slightly lower than the 7% growth rate during each of the past two years. In the early 2000s, employers and workers suffered through a sustained period of low double-digit rate increases, making recent numbers look relatively manageable, said Altman of KFF.
Yet the absolute dollars being spent on worker health insurance are big, he said, and getting bigger.
“I am not predicting a return to low double-digit increases, but it would not shock me,” Altman said. “Employers have nothing new to throw at the problem, and that could result in a new wave of increasing deductibles and other forms of employee cost sharing, the tried-and-true strategy that neither employers nor employees like.”
Total health benefit costs per employee next year are expected to rise at the fastest rate in 15 years, according to a report last month from New York-based Mercer that uses a different methodology.
KFF’s survey found that about 1 in 5 large firms offering health benefits said they are covering costly GLP-1 drugs such as Wegovy for weight loss.
The class includes the well-known brand Ozempic, for people with type 2 diabetes managing blood sugar levels.
Among firms with at least 5,000 workers, 43% said they were paying for the weight loss medications in their largest health plan, up from 28% in 2024.
Employers often put conditions on coverage of the medications, but KFF found use has been higher than expected.
“While recognizing their effectiveness in addressing obesity, many employers indicated they were considering scaling back coverage,” KFF researchers wrote in a companion report being released Wednesday.
Obesity is associated with many serious and costly health problems such as cardiovascular disease and cancer, making it one of the most serious health issues for the nation given its large and growing incidence.
There are hopes that GLP-1 drugs eventually will deliver savings in terms of decreased costs for other health conditions, but any such benefits aren’t uniformly clear yet to employers, said Matthew Rae, an associate director with KFF.
The analysis is complicated, Rae added, since some workers as they lose weight might start using more services like knee replacement surgery, for which their weight previously made them ineligible.
“I don’t think we’ve totally sorted this question out yet,” he said.
While family coverage in employer-sponsored health plans is nearly $27,000, the average annual premium for single coverage is $9,325, up 5% over last year.
Nearly three-quarters of people with single coverage face an annual out-of-pocket maximum of more than $3,000. This upper limit on spending exceeds $6,000 for about 1 in 5 people with single coverage.
“While key measures such as the average deductible have grown more modestly in recent years, continued premium growth could prompt employers to raise out-of-pocket amounts for workers,” researchers wrote. “Yet many may feel constrained in doing so ... (because) many covered workers already face substantial cost-sharing.”
©2025 The Minnesota Star Tribune. Visit at startribune.com. Distributed by Tribune Content Agency, LLC.







Comments